Interprofessional Education Curriculum Repository
Interprofessional education for trainees and practicing health professionals is a key step in realizing the benefits of interprofessional collaborative practice (ICP). Collaborative practice is the provision of health care services that emerge from and rely on the knowledge and skills of 2 or more health or social care providers. ICP is a specific form of teamwork that has been shown to improve healthcare delivery and outcomes in many different settings and for many different populations. This repository features resources on Interprofessional Collaborative Practice and are accessible through INDIGO, a free digital repository supported by the University Library.
Interprofessional Collaborative Practice Videos Heading link
This 5-part video series will help early learners (students and practitioners) develop foundational knowledge for understanding interprofessional collaborative practice and develop interprofessional practice skills. The video series is comprised of the following videos below.
- Collaborative Practice Contributes to Improving Healthcare: This video covers the definition of ICP and the forces driving the focus on ICP.
- Conceptual Frameworks for Interprofessional Collaborative Practice: This video includes an overview of the IPEC Core Competencies for Interprofessional Collaborative Practice, the IHI Triple Aim Framework & the Quadruple Aim, and the International Classification of Functioning, Disability, and Health.
- Making Interprofessional Collaborative Practice a Reality: This video covers some of the barriers and facilitators of interprofessional collaborative practice.
- Core Competencies for Interprofessional Collaborative Practice: This video covers the IPEC Core Competencies for Interprofessional Collaborative Practice and provides some example applications to practice
- Team Science in Healthcare: This video describes what makes a team effective using Eduardo Salas drivers of team effectiveness.
Patient Cases Heading link
The patient cases were developed for students to work in interprofessional facilitated teams to discuss the ways in which IPEC core competencies could enhance the patient’s case and improve the delivery of care to the patient (Interprofessional Education Collaborative (2016)Washington, D.C.).
Barbara Smith

Barbara Smith is a 72-year old woman who is admitted to the hospital through the emergency department, following a fall in her home. She has surgery to repair a hip fracture and stays in the hospital for eight days.
There are 4 videos that highlights Barbara Smith’s experience from emergency to home health discharge:
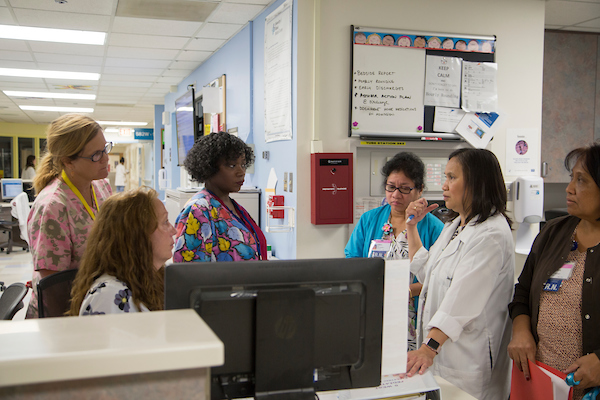
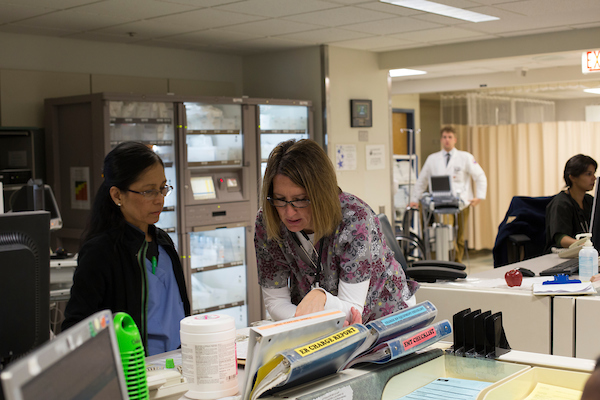
- Video 1: Barbara Smith’s visit to the emergency department
- Video 2: Barbara Smith’s interprofessional discharge planning meeting in the acute care unit
- Video 3: Barbara Smith’s interprofessional home health discharge conference (short version)
- Video 4: Barbara Smith’s interprofessional home health discharge conference (long version)
Suggested Debriefing
Objectives: Barbara Smith’s Visit to the Emergency Department Video
- Describe the roles and responsibilities of each discipline in this ED scene, based solely on the information extracted from the scene.
- Describe where roles were complementary, overlapping and unique.
- Assess each care provider’s communication style and approach to the patient and daughter.
Suggested Debriefing: Small Group Questions
- Can you identify all of the team members who talked to Barbara Smith? Is there any overlap between the roles of the team members involved?
- What are the impressions you had about the team members’ roles and interactions with Barbara? Did anything you saw challenge any preconceptions or stereotypes you may have held about specific disciplines?
- e.g., How did you judge roles of team members (physical characteristics such as clothing, leadership style, tone of voice, language used, etc)? Who were you surprised to see as a member of the team or as absent from the team? Any other behaviors surprise you? Anything that you learned about these roles that you didn’t know prior to this workshop?
- Describe the communication style between the team in the hallway (e.g., Do they demonstrate active listening to each other? Do they share information with each other in a respectful manner that encourages collaboration and joint decision-making in care? Is this typical to see all members gather together to discuss patient care?)
- When Crystal joined the discussion in the hallway, what indicated that she was an accepted member of the team?
Examples of Key points to highlight in discussion:
- Patients encounter a good number of people from different professions who have different roles – it is important to introduce yourself including who you are and why you are there.
- It is important to avoid discipline-specific terminology and if used, then define it in an understandable manner
- Verbal and nonverbal behaviors convey respect and offer support to other team members regardless of health profession or status (e.g., challenging due to the social hierarchy in place within health professions)
- Crystal was asked to assist in convincing Barbara to be admitted for surgery – this was okay because she was in agreement with the team
Suggested Debriefing
Objectives: Acute Care Unit Video
- Describe the roles and responsibilities of each discipline in this Acute Care Unit scene, based solely on the information extracted from the scene.
- Describe the specific strategies and actions team members used to verify the patient’s and daughter’s understanding and ensure that the decision made by the patient and daughter was well informed.
Suggested Debriefing: Small Group Questions
- Describe the communication style between the team and the patient. Provide examples of effective verbal and non-verbal communication strategies/techniques. (e.g., Do they engage in active listening with the patient and daughter? Do they ask the patient and her perspectives? Do they provide clear explanations for recommendations? Do they address the patient’s questions? Do they respect that Ms. Smith is the patient and has full decision making authority in her care?)
- Discuss how this approach in communication can impact patient care (e.g., facilitates the development of a trusting relationship with team members, patients, families; provides effective transfer and sharing of information).
Example of Key points to highlight in discussion:
- Acknowledgement of all disciplines represented in team and clear explanation of how they work as a team to provide care
- Use of effective verbal and nonverbal behaviors to convey respect and offer support to patient and daughter (e.g., good eye-contact, positive and empathetic tone of voice, appropriate and encouraging facial expressions)
- The team recognized that Barbara’s desire to go home was in conflict with what they felt was in her best interest.
Suggested Debriefing
Objectives: Home Health Discharge Video
- Describe the roles and responsibilities of each discipline in Barbara’s discharge planning conference.
- Assess each clinician’s communication style and ability to respectfully and effectively communicate findings and address the different perspectives of the patient/daughter and the team.
- Identify how the complexity of the health care system specifically related to transitions between settings (home, ED, acute care) creates challenges to safe, respectful and effective patient centered care
Suggested Debriefing: Small Group Questions
- Describe the roles and responsibilities of each discipline—was the team able to adopt a patient-centered approach?
- Discuss each clinician’s communication style and ability to respectfully and effectively communicate findings.
- Discuss and address the different perspectives of the patient/daughter and the team.
- How is the complexity of the health care system specifically related to transitions between settings (home, ED, acute care) create challenges to safe, respectful and effective patient centered care.
Example of Key points to highlight in discussion:
- Team ultimately wants to feel like they gave the patient the right content and amount of information – but then the patient/caregiver decides.
- Transitions between care settings are potential trouble spots.
George Jones Heading link
The next set of videos features George Jones.
George Jones
George Jones is a 53-year-old male who comes to his primary care provider’s office with a recurring complaint of back pain for which he wants a prescription refilled.
In the first video, the nurse and nurse practitioner he sees are concerned about lack of follow up with referrals to physical therapy and occupational therapy and about possible substance use disorder. In the next two videos, George is going through an intake evaluation in a team based chronic pain management program. One video shows an idealized team interaction and the other video shows flawed team interaction.
- Video 1: Primary Care Office Visit
- Video 2: Initial Visit to the Pain Clinic – Version 1 (flawed team interaction)
- Video 3: Initial Visit to the Pain Clinic – Version 2 (idealized team interaction)
Questions to Consider
As you watch George’s experience at the pain clinic, please reflect on the following:
- What did the clinician’s do well?
- How do you think the clinicians could have improved George’s experience?
- How would you like to see your professional role represented in advancing George’s patient centered care? How would you like to see an interprofessional health care team represented in advancing George’s patient centered care?
Healthcare Professions Videos Heading link
A lack of understanding of knowledge and skills of other members of the team inhibit teamwork and it is frequently mentioned by current practitioners as a barrier to effective teamwork. This section provides information about the roles and responsibilities of a profession as well as the training it takes to carry out those roles and responsibilities. For each profession, there is a brief video – less than 10 minutes each. This site will be updated with additional profession videos in the coming months.
-
Dentistry

This video prepares all members of the health care team to collaborate with dentists. This video provides an overview of the roles and responsibilities of dentists in the US Health Care System, the educational preparation for a career in dentistry, challenges facing the dental profession, and future developments in dentistry.
-
Nutrition

This video prepares all members of the health care team to collaborate with dietitians. The video provides an overview of the roles and responsibilities of dietitians in the US Health Care System, the educational preparation for a career in nutrition, challenges, and future developments in the profession.
-
Social Work

This video prepares all members of the health care team to collaborate with individuals in the social work profession. The video provides an overview of the roles and responsibilities of social workers in the US Health Care System, the educational preparation for a career in social work, challenges, and future developments in the profession.
-
Public Health

This video prepares all members of the health care team to collaborate with public health professionals. The video provides an overview of the roles and responsibilities of public health professionals in the US Health Care System, the educational preparation for a career in public health, challenges, and future developments in the profession.
-
Health Information Management

This video prepares all members of the health care team to collaborate with health information management professionals. The video provides an overview of the roles and responsibilities of health information management professionals in the US Health Care System, the educational preparation for a career in health information management, challenges, and future developments in the profession.
-
Pharmacy

This video prepares all members of the health care team to collaborate with pharmacists. This video provides an overview of the roles and responsibilities of pharmacists in the US Health Care System, the educational preparation for a career in pharmacy, challenges facing the pharmacy profession, and future developments in the profession.
-
Physical Therapy

This video prepares all members of the health care team to collaborate with physical therapist. This video provides an overview of the roles and responsibilities of physical therapists in the US Health Care System, the educational preparation for a career in physical therapy, challenges facing the physical therapy profession, and future developments in the profession.
-
Medcine
This video prepares all members of the health care team to collaborate with individuals in the Doctor of Medicine profession. The video provides an overview of the roles and responsibilities of physicians in the US Health Care System, the educational preparation for a career in medicine, challenges, and future developments in the profession.
-
Nursing
This video prepares all members of the health care team to collaborate with individuals in the Nursing profession. The video provides an overview of the roles and responsibilities of nurses in the US Health Care System, the educational preparation for a career in nursing, challenges, and future developments in the profession.
-
Profession Video: Occupational Therapy
This video prepares all members of the health care team to collaborate with individuals in the Occupational Therapy profession. The video provides an overview of the roles and responsibilities of occupational therapists in the US Health Care System, the educational preparation for a career in occupational therapy, challenges, and future developments in the profession.
IPE Facilitator Training Heading link
Facilitators play an important role in the successful development of collaboration-ready professionals. This section features a series of IPE facilitation training modules. Facilitators will acquire foundational knowledge about interprofessional team facilitation through independent study and reflection.
Module 1: Facilitation Fundamentals
Module 1 provides an introduction to the role of a learning group facilitator. It introduces key facilitation skills and practical considerations. This module is designed for novice facilitators who are working on developing their facilitation skills.
At the end of this module, you will be able to:
- Describe the role of a Learning Group Facilitator.
- Describe the fundamentals of facilitation to ensure a safe environment for a learning group.
- Describe common facilitator responses and actions in the learning process.
Module 2: Effective Feedback Process
Providing timely, specific, and actionable feedback has a powerful impact on the quality of the students’ learning process. This module reviews key principles of good feedback practice. This module is designed for all facilitators, experienced or novice.
At the end of this module, you will be able to:
- Describe the elements of effective feedback.
- Describe the significance of supporting self-efficacy in the feedback process.
- Describe the feedback process.
- Apply fundamentals of facilitation to provide feedback using the coaching feedback process.